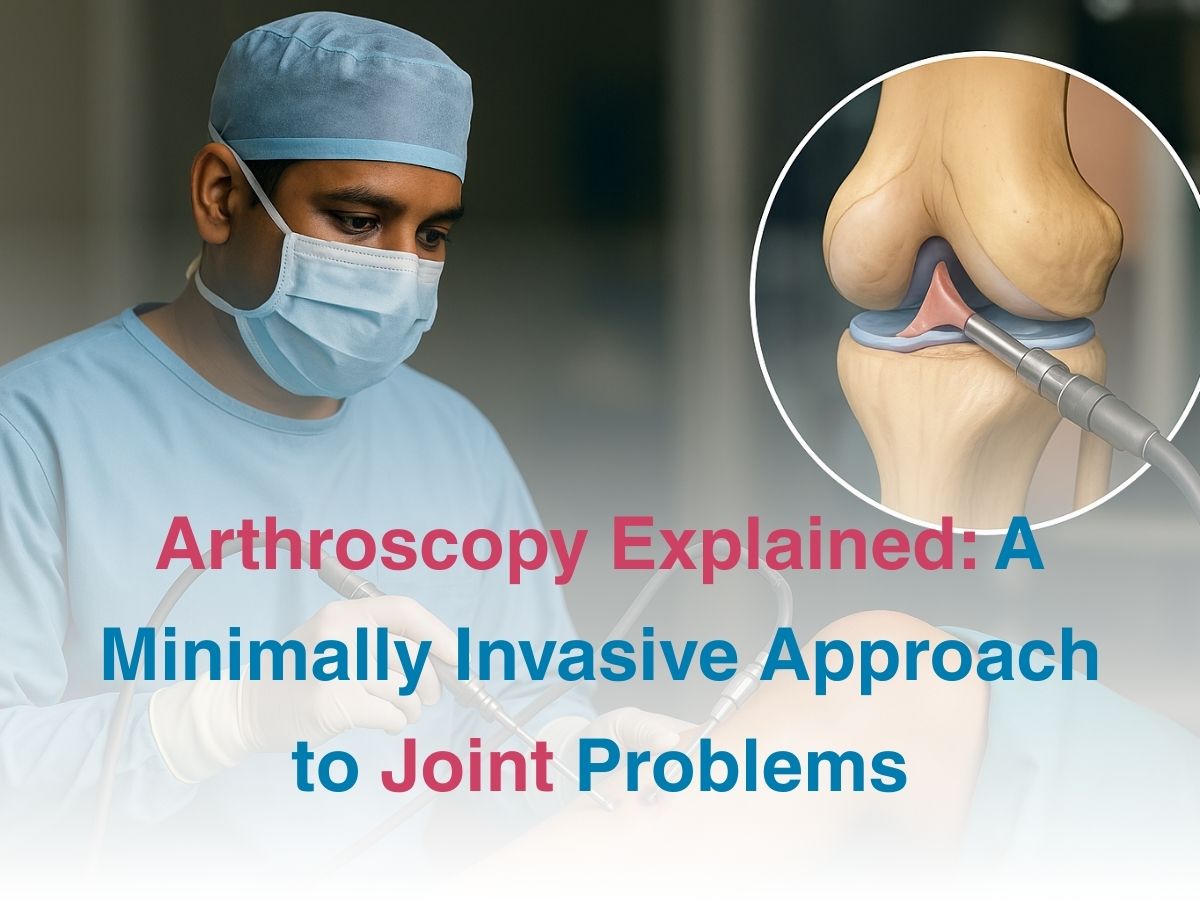
Arthroscopy Explained: A Minimally Invasive Approach to Joint Problems
Minimally Invasive Knee Arthroscopy Benefits
Modern arthroscopy has gently overturned fear, offering a technique where instead of cutting open the knee in its entirety, surgeons now rely on tiny entry points, guiding delicate instruments that can mend torn ligaments and smoothen rough cartilage. Since the surrounding tissues and muscles are spared from unnecessary trauma, the outcome is not just a smaller scar but also less pain and faster discharge.
Ankle Arthroscopy Post-Operative Care Instructions
The ankle, though smaller and often overlooked in discussions of major joints, is no less important, for it is the unsung hero of balance and movement, adjusting to uneven pavements, sudden potholes, festive dances and long walks on crowded Indian streets. When it gives way to injury, either due to ligament tears, cartilage lesions, or chronic swelling – ankle arthroscopy comes into play as a minimally invasive method of repair. But the story does not end with surgery itself because post-operative care is the true determinant of recovery. Here, discipline becomes the patient’s closest ally, with doctors usually advising strict leg elevation to reduce swelling and keeping the surgical site clean and dry until the wounds heal. Mobility is reintroduced in carefully measured stages, often with crutches to share the load initially, followed by guided physiotherapy to restore strength, balance, and flexibility respectively.
Complications and Risks of Joint Arthroscopy Surgery
Every medical advance, however celebrated, carries its own shadow and arthroscopy, despite its reputation as a minimally invasive marvel, is no exception. It is still a surgical intervention with potential risks and while the likelihood of severe complications is low, they must still be acknowledged. These can range from infection at the incision site to excessive bleeding, blood clots, or accidental damage to surrounding structures. Even though the incisions are small, stiffness, residual pain, or incomplete resolution of the original problem can occasionally follow. Finally, it is also really important to note that NOT everyone is a good candidate for minimally invasive surgery.
Conclusion
Arthroscopy in its truest sense, is not merely about smaller cuts or quicker healing alone. It quietly redefines joint care, turning what was once an ordeal into a manageable step on the path to better health. When we call it minimally invasive, what we really mean is that it is maximally enabling, giving back not just function but confidence, dignity, and freedom – qualities that no scar, however small or large can ever measure. We live in a society where every step matters- from walking to working, to standing in queues or participating in festivals; so, the return of untroubled movement is nothing less than a gift – one that modern medicine has now placed within easier reach