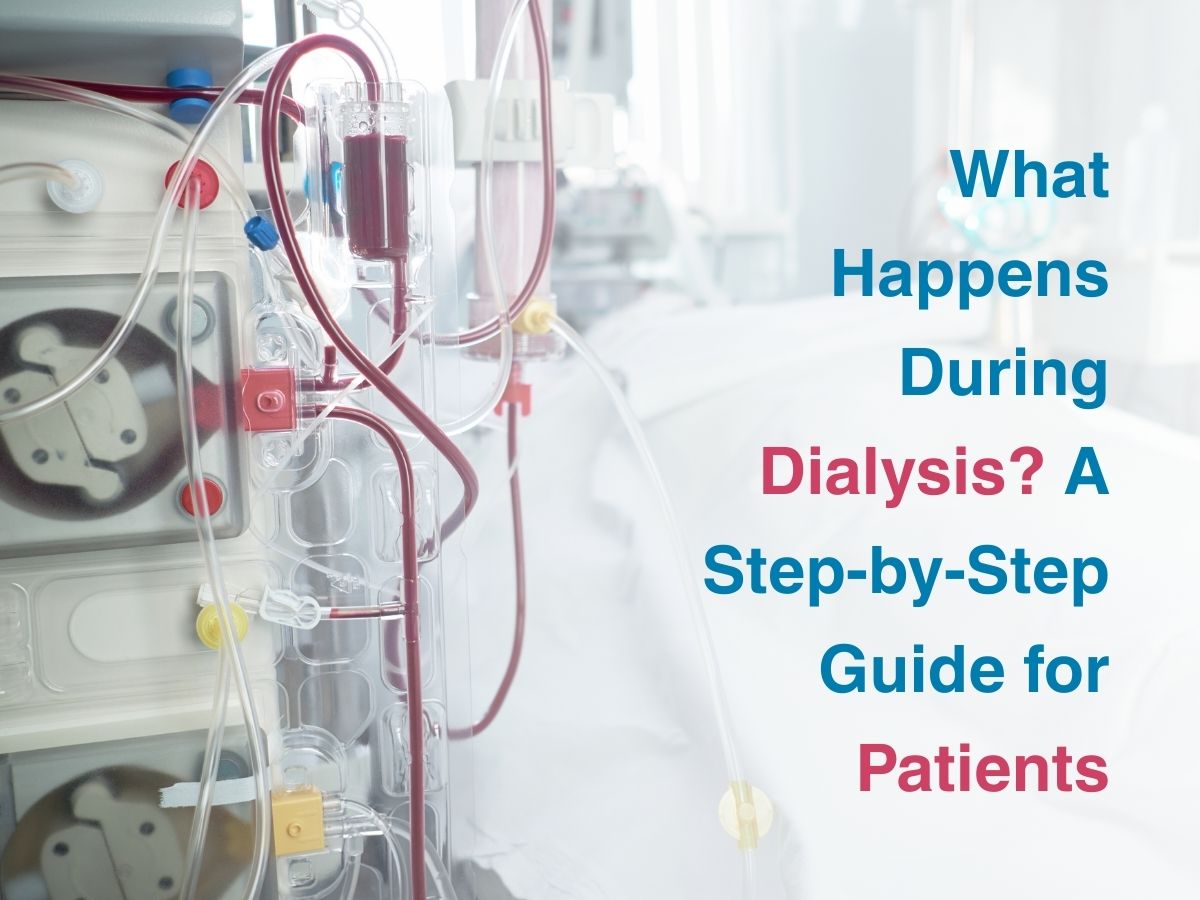
What Happens During Dialysis? A Step-by-Step Guide for Patients
What Happens To The Body During Dialysis?
Dialysis is like an external caretaker, diverting blood through a machine that gently removes excess water, urea, potassium and waste that your kidneys can no longer manage, returning the cleansed blood back to you, helping you feel lighter, less fatigued and more clear-headed.
During the process, toxins that build up in the blood are drawn into the dialysate fluid through semipermeable membranes. Excess fluid leaves via ultrafiltration and the balance of sodium and other electrolytes is delicately corrected, which means your blood finds renewed balance while invisible weight from fluid retention is lifted.
How Does Dialysis Machine Work For Kidney Patients?
If you picture a dialysis machine as part engineer’s lab, part healer’s companion, you’re close- because it receives your blood, pumps it through intricate tubing, carefully temperature-controls it, passes it beside a countercurrent of clean, specially composed fluid (dialysate) and through its membrane filters allows waste and excess salts to exit, while returning purified blood to your body. Sensors monitor pressures, volumes and flow throughout this delicate process.
What Dialysis Feels Like For First-Time Patients?
A first dialysis session may feel like stepping into a slow-moving river, where initial unease from needles or unfamiliar noises gradually turns into rhythmic acceptance, as the machine becomes a steady breath beside you. While the initial pricks bring tension and the hum of pumps feels unnerving, soon you may settle into a kind of trance- your thoughts drifting between hopes lost and hopes revived, as pauses feel like they are filled with the hum of life’s pulse through tubes and filters.
By the end of that first session, most patients describe a surprising clarity- mental fog lifts, breaths become easier, limbs less burdened by heaviness- though some feel tired or lightheaded briefly and those responses are the body’s way of acclimating to the new rhythm of purification that has become, for many, a quiet companion in their healing circuit.
Diet And Precautions Before And After Dialysis
Navigating food around dialysis requires a gentle balancing act- too much potassium in bananas or greens can amplify heart strain; too much phosphorus in dairy and legumes can weaken bones; too much fluid can accumulate where kidneys can’t bail it out- hence patients often learn to rotate foods mindfully: enjoying cauliflower and apples, measured milk intake or chikkis, while reducing high‑salt pickles and keeping an eye on fluid intake from drinks, soups and rasam.
Before dialysis, avoiding a heavy meal helps prevent queasiness or nausea on empty or spinning stomachs during sessions- which is why some prefer a slice of toast and water beforehand, while post‑dialysis many savour a light warm dal, chapati and colourful vegetables that refuel without tipping sodium or fluid balance. Such meals are designed to nurture strength without disturbing the body in any major way.
Practically, carrying a home‑prepared lunch, asking for low‑salt soups, pacing fluids by sipping, and reminding oneself that each oral intake is part of blood balance and not indulgence can empower patients to take nutrition into their own hands, shaping the invisible support that complements the machine’s effort each week.
Conclusion
Dialysis is not just a medical process- it is a tender partnership between machine, medical team and body, where each session becomes a healing hum that lifts weight, clears toxins and buys time for patients to breathe, work, care, laugh again- deeply and confidently. In every drop of blood filtered and every cautious meal chosen, dialysis becomes more than a treatment- it becomes a testament to resilience, a renewal of trust in life’s rhythms and a vivid reminder that healing can indeed flow through tubes and tender practices, restoring strength inside and out.